by Elise Wachspress
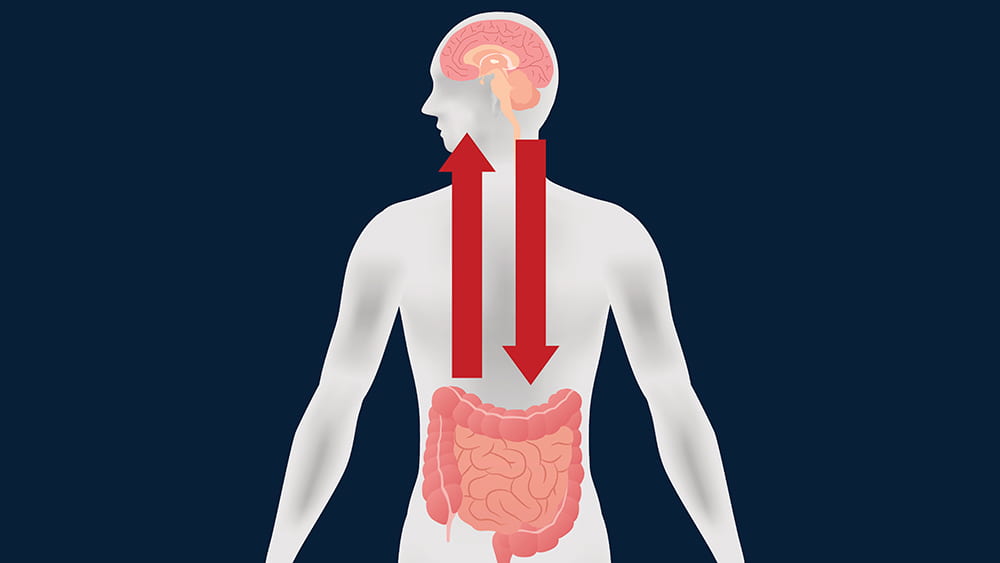
If you read the news—or this blog—then you know that researchers are identifying more and more interactions between the brain and the gastrointestinal tract. Some of these linkages are directly neurological; many others are chemical interactions caused by digestive byproducts of the bacteria in our guts.
A large group of scientists from the University of Chicago (led by Issam Awad, MD), the University of Pennsylvania, and universities and academic medical centers from New York to San Francisco and Australia to Germany have found another mechanism on the path from the gut to the brain—and with it, perhaps a new way to intervene in diseases that affect the most inaccessible organ of our bodies. Their report was the cover story of Science Translational Medicine this past November.
The story starts with decades of research on a rare condition, cerebral cavernous malformations (CCM). CCM causes enlarged, irregular clusters of capillaries, the tiniest blood vessels. CCM capillaries have abnormally thin walls, without the elastic fibers that make the vessels pliable. These irregularities, which make the vessels prone to lesions and blood leakage, can occur throughout the body. But they are by far most worrisome in the brain and spinal cord, where the leaks can lead to seizures, stroke, hearing or vision loss, even paralysis.
CCM is caused by genetic mutations in one of three different genes, but one of these is not like the others. Patients with mutations in the PDCD10 gene usually suffer much earlier, more severe health events, like brain hemorrhage.
A disorder with such disastrous outcomes linked so closely to single gene mutations encouraged researchers to develop mouse models for each of the three mutations. The models could help them discover the molecular mechanisms involved in each—especially what was different in the PDCD10 mice—and exploit what they learned to develop new treatments and preventive measures for CCM.
But examining the brain slices of the mice under the microscope was expensive and time-consuming. An Australian colleague noted that he had heard of instruments that could do x-ray microcomputed tomography on tiny subjects. Awad discovered only one in the entire Midwest, which happened to be in the basement of ivy-covered Culver Hall, one of the oldest buildings on the UChicago campus. Evolutionary paleobiologist Zhe-Xi Luo, PhD had acquired this microCT (now dubbed a Paleo CT!) to examine tiny, delicate insect fossils. A partnership was born, and, with Luo’s support, Awad’s team had a much faster way to assess precisely the amount of bleeding in each mouse brain and the correlation with various genetic, dietary or pharmacologic manipulations.
The investigators found that mice that developed disease did, in fact, share a characteristic microbiome. These bacteria produced a lipopolysaccharide—often called an endotoxin—on their outer membranes, a likely culprit in fostering disease progression. But the fact that the microbial communities were similar among all three genetic models indicated that it wasn’t the microbes alone that made mutant PCDC10 so much more virulent than the other two mutations.
The team moved on to test whether the PDCD10 mutation might cause some kind of rupture in the mucus membranes coating the gut, and there they found the smoking gun. The mutant gene did, in fact, attack the gut’s mucus layer, allowing the offending microbes access to the deeper tissues of the colon. With the integrity of the gastrointestinal tract compromised, bacterial byproducts could leak into the mice’s blood stream and be carried to the brain.
Awad’s team is currently extending this research in mice to patients with CCM. They hope to see how the microbiome can be used as a biomarker of disease and how targeting therapies to the gut might prevent brain bleeding. In the meantime, they think CCM patients might want to avoid polysorbate 80. They might also try any conditions or foods—or drugs—that foster mucus production, which might be helpful in preventing further degradation not only in the gut, but also the capillaries in the brain.
There are implications for the rest of us. The Awad team has found genetic anomalies in the aging brain similar to those in CCM. So what they learn about the mechanisms of this rare disease might also be used to prevent brain bleeding in the rest of us as we age. By carefully manipulating PDCD10 and the mucus layers of the gut, we may one day learn how to better care for what is arguably the most important and delicate organ in the body—the brain.
Elise Wachspress is a senior communications strategist for the University of Chicago Medicine & Biological Sciences Development office