by Tim McGovern
Writer and editor based in Chicago
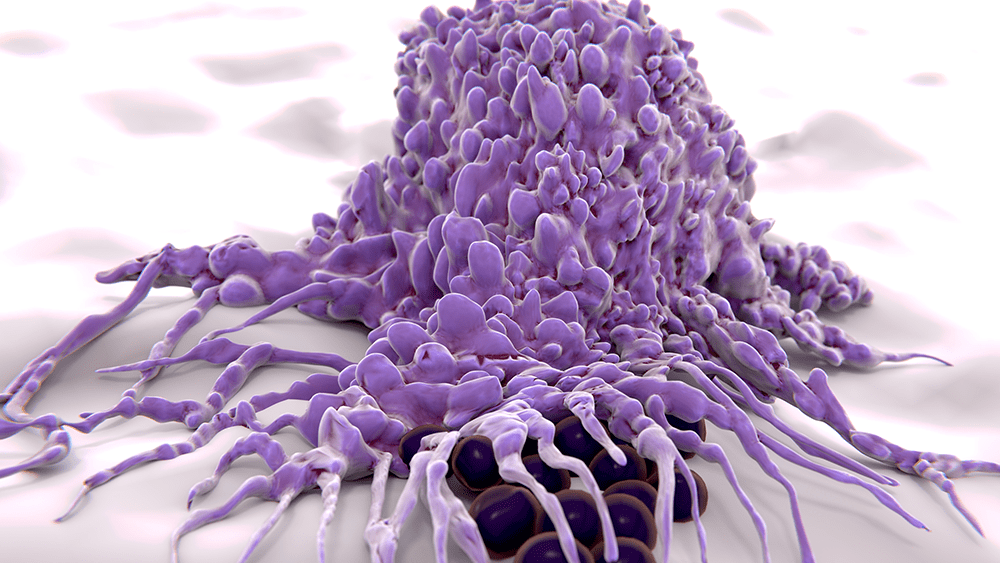
Remember The Blob? Even if you’ve never seen this 1958 B-movie classic, pop culture has likely introduced you to the concept: a shapeshifting mass that extends to swallow up and dissolve its enemies. This swallow and dissolve approach—on a microscopic level—is how white blood cells deal with infections. As Lev Becker, who specializes in these cells, explains: “These macrophages (their very name means ‘big eaters’) and neutrophils (the ‘first-responder’ white blood cells) are in every tissue in your body, and they play a fundamental role in maintaining your health, protecting you against infections from viruses or bacteria.”
Unlike the Blob and its strategy of indiscriminate destruction, white blood cells do a pretty good job of distinguishing the “good guys”—healthy human tissue—from the “bad guys”—viruses and bacteria. But sometimes they get it wrong. Becker goes on: “If they’re chronically incorrect—for instance, over-inflamed in the context of diabetes and heart disease, or under-inflamed in the context of cancer—long-term illnesses can result. And although we are looking at a variety of diseases, what unifies our lab is the philosophy and approach that one can either activate or inhibit the innate immune system to treat human disease.”
To understand how immune cell activity plays out in human disease, Becker and his team use an array of leading-edge techniques. “We always start with people,” he says, “and ask ‘What is different in the cells of people with and without a given disease?’ Then we work to find mouse models and cell systems that replicate that dysfunction.” This approach sets his lab apart from a more “traditional” approach: start with a molecule and learn everything about it in the cellular context, then—if it seems the molecule might play a role in disease—develop a mouse model, and finally, if the mouse results are promising, figuring out a way to ascertain the molecular activity in humans.
In Becker’s lab, “Every project has a human, mouse, and cell component to it.” It takes a novel assortment of tools to work in this way. In addition to the core biochemistry the team employs to parse the molecular pathways, they have developed new assays using cutting-edge computational techniques, with the goal of understanding the entire range of protein activity in a given cell. The capstone to all this molecular research is the lab’s ability to test their hypotheses not only in petri dishes, but in mice and human patients.
This ability to take research from human to molecule to human was always part of Becker’s plan: “My initial thought going into basic science versus medical science is that to impact health you have to take it one step further. Research scientists always hope that one day their findings will lead to treatments, but our focus on the translation part of research is especially important to us. We want to create medical interventions and develop therapeutics. That’s where we’re trying to go: start with humans, go back, find a molecule, take it to mice, and then launch a company, get funding, and move forward with actually developing and testing a therapy.”
A couple of years ago, leveraging the expertise and resources of the University’s Polsky Center for Innovation and Entrepreneurship, Becker launched Onchilles Pharma Inc. With seed funding from the George Shultz Innovation Fund, Onchilles is working to bring Becker’s research back to people, in the form of cancer immunotherapies which are more powerful, more precise, and better tolerated than current treatments.