by Elise Wachspress
Through the many posts on the WellNews blog, we’ve pointed out correlations between diet and disease, microbial diversity and wellness, sleep and neurological health. Science often progresses via experiments in which one variable is tested against one outcome, a binary approach that allows us to make definitive statements about causations—or at least correlations—between pairs of conditions.
But life—and our body systems—are messy. There are countless variables involved in keeping the human machine functioning. For starters: over 20,000 genes determine our body plan, direct the assembly of the proteins that power our cells, and lay out the immunological system that protects us from foreign intruders. Then there are the trillions of molecules in the air, water, soil, and food that we take in every day which can activate or deactivate those genes. There are the variables of temperature and sunlight, affecting our sleep cycles and how we manufacture our vitamins.
And there is the impact of the bacteria—more numerous than all our cells—with whom we share our bodies.
In this amazingly complex ecosystem, everything affects and is affected by everything else.
Recently, the world has been gob-smacked by another player in the human ecosystem: viruses. The virus COVID-19 is exerting an outsize influence on international travel, the supply chain, the economy, and the governments of China and Singapore, as well as the news media. The virus, really just a packet of molecules—not even really alive—is hard to detect until it has successfully infected cells. Now the global race is on to understand the “strategy” COVID-19 uses to get into our cells and replicate, often causing significant distress and sometimes death.
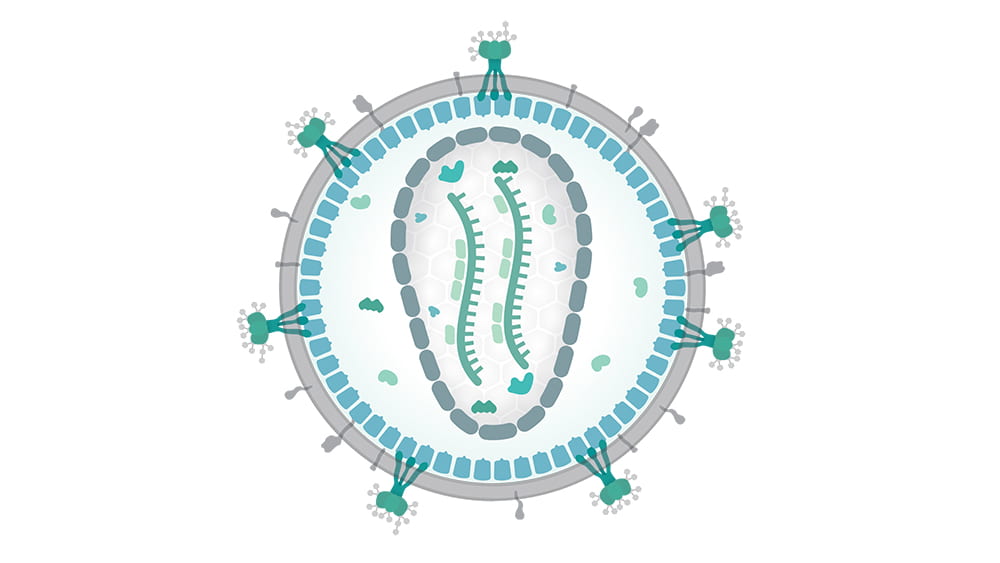
Not so long ago, another type of virus—the human immunodeficiency virus, or HIV—initiated similar havoc. HIV is a retrovirus, a packet of RNA that inserts itself directly into cell genomes, and once inserted into cell DNA, continues replicating through generations of cells.
Tatyana Golovkina, PhD, is an expert in retroviruses, how the immune system detects and attempts to neutralize them, and how the retroviruses fight back. In important research nearly a decade ago, Golovkina and her team demonstrated that retroviruses use certain normal bacteria (some on the mucus membranes, others from the gut) as a kind of Trojan horse to get themselves inside the body. Once inside, the retroviruses stimulate a specific immunosuppressive protein, and with the immune system’s guard down, start invading cells and getting themselves reproduced.
Understanding how retroviruses operate is an important step in resolving multiple diseases. Some retroviruses carry cancer-causing genes in their RNA; some integrate themselves into cells primed with mutations and tip them into cancer. Other retroviruses can trigger neurological and neurodegenerative disorders.
To understand how retroviruses operate, Golovkina and her team use specialized, inbred mice that are naturally resistant to some retroviral infections. In these animals, the viruses can gain entry into the cell, but can’t get their RNA inserted into the cell’s DNA. That’s because the mouse’s cells produce a substance—an antibody—which coats the outside of the viral RNA packet, keeping its payload isolated from the cell nucleus.

Photo credit: Daniel Beyer/Wikimedia Commons. Translated by Raul654. CC BY-SA 3.0 – https://creativecommons.org/licenses/by-sa/3.0/deed.en
Golovkina’s work with these mice has already provided significant information that could help us fight retroviral infections. She has identified the single locus—the exact place in the genome—with the instructions for making the mouse’s antibody-coating factor… and it turns out that humans have an analogous gene. Her team has also found a receptor in the mouse immune system that detects the retrovirus and signals the body to make the antibody… and it just so happens that humans have an analogous mechanism, known to detect HIV. So the team has found both a potential target for treatment and an avenue for signaling that target.
More important, they’ve found this antiviral system is present and active from the day the mice are born.
Long experience has shown that babies are best vaccinated several weeks or months after birth, when their immune systems are more fully developed. But we also know that AIDS and other retroviruses can be passed from mother to newborn during birth and breastfeeding. Golovinka’s studies of how mice repel viral attacks can help devise inoculation strategies that protect these babies, as well as adults, from HIV and other retroviruses. It may also help address non retroviruses, like hepatitis, that share some similar mechanisms.
While the complexity of the human system sometimes feels overwhelming, discoveries like these and scientists like Golovkina are, step by step, providing the knowledge we need to live happier, healthier lives.
Elise Wachspress is a senior communications strategist for the University of Chicago Medicine & Biological Sciences Development office
Main photo credit: Thomas Splettstoesser/Wikimedia Commons (CC BY-SA 4.0)