

Understanding the β cell in Diabetes
Diabetes is reaching epidemic proportions in the USA. A recent analysis revealed that the prevalence of pre-diabetes and diabetes in the US is in excess of 50%. Both major forms of diabetes, type 2 (T2D) and type 1 (T1D), are increasing in incidence in the USA. Similarly, it is becoming increasingly apparent that both forms of diabetes share cellular pathogeneses, where dysfunction and/or death of islet β cells is a common denominator. To that end, the Mirmira Lab is focused on understanding the specific role of the β cell during the pathogenesis of diabetes. Our laboratory has been focused on diabetes research for the past 20 years. Our lab has been host to high school students, undergraduates, graduate students, and postdoctoral scholars over these years, and more 50 people have trained in our lab and have gone on to careers as scientists, physicians, and educators. You can learn about our research and the members of our laboratory on this website. If you want to learn more about our lab and the research, contact us.
Research Areas

Lipoxygenase Pathway
12/15-lipoxygenase catalyzes the oxygenation of fatty acids to produce lipid pro-inflammatory mediators, the primary being 12-HETE. One of our initial studies showed that the deletion of 12/15-lipoxygenase in the pancreas is sufficient to protect against obesity-induced glucose intolerance, via a mechanism involving Nrf2-mediated activation of antioxidant genes (Tersey et al. MCB 2014).
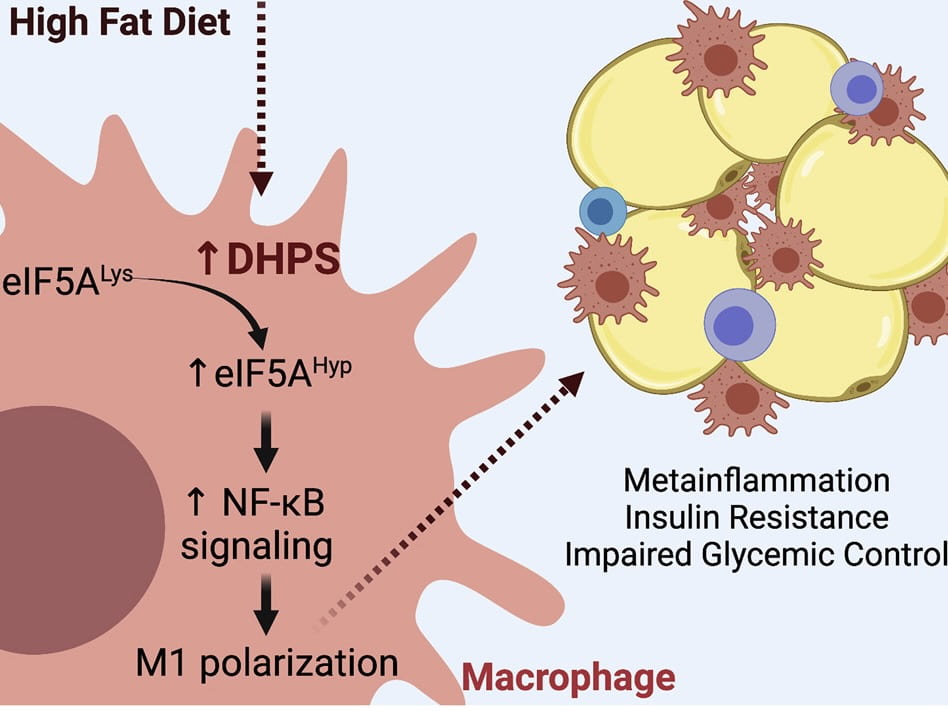
Polyamine Pathway
Pancreatic β cell proliferation is significantly reduced in adults. Interestingly, during the early phases of diabetes, the proliferative capacity of the β cells is increased, possibly for adapting to the increased insulin demand. Our lab has previously shown that the translation factor eIF5A acts as a sensor that catalyses the translation of mRNAs involved in cellular replication.

Biomarkers
Type 1 diabetes (T1D) is a complex and heterogenous disease. Insulin-producing β cells are the target of destruction by the immune system, and those who display autoantibodies against β cell antigens are at highest risk for developing the disease. Development of autoantibodies is a relatively late event in the pathogenesis of the disease, and recent studies using immune-suppressive agents in these individuals delays the onset of diabetes, but does not prevent it.
Lab News
Upcoming Events & Opportunities
UChicago Endocrine Research Seminars
2025 – 2026 Speakers
October 6, 2025: Dr. Christoph Buettner, Rutgers
October 13, 2025: Dr. Sarah Tersey, The University of Chicago
October 27, 2025: Dr. Scott Soleimanpour, University of Michigan
November 10, 2025: Dr. Andrew Koh, The University of Chicago
November 17, 2025: Dr. Mudassir Rashid, Illinois Institute of Technology
December 1, 2025: Dr. Yuwei Jiang, UIC
January 5, 2026: Dr. Lisa Beutler, Northwestern
January 12, 2026: Dr. Klara Klein, UNC
February 2, 2026: Dr. Kristen Knutson, Northwestern
February 9, 2026: Dr. Dario DeJesus, The University of Chicago
February 23, 2026: Dr. Liana Billings, Northshore
March 9, 2026: Dr. Grant Barish, Northwestern
March 16, 2026: Dr. Nadia Bozadjieva-Kramer, University of Michigan
March 23, 2026: Dr. Congcong He, Northwestern
March 30, 2026: Dr. Suzanne Devkota, UCLA
April 20, 2026: Dr. Marie-Pierre St. Onge, Columbia
April 27, 2026: Dr. Barbara Kahn, Harvard
May 4, 2026: Dr. Christine Yu, St. Jude
May 18, 2026: Dr. Megan Prochaska, The University of Chicago
June 1, 2026: FELLOWS: Dr. Anne Gandolfi and Dr. Hansika Narayanan
June 22, 2026: FELLOWS: Dr. Victoria Wang, Dr. Kareem Al-Qadi, Dr. Caroline Abe, and Dr. Fawsia Osman
June 29, 2026: FELLOWS: Dr. Kerim Kaylan, Dr. Rachel Umans, and Dr. Jeremy Winer


