May 29, 2019 | Microbiome, Neuroscience, News Roundup
A selection of health news from the University of Chicago and around the globe curated just for you.
Improving care for young hearts
Ivan Moskowitz is investigating the genetic causes of pediatric congenital heart disease (CHD) in an effort to improve diagnosis and treatment of children born with this condition. A recent gift from The Heart of a Child Foundation will help support his research. (Give to Medicine)
Antibiotic treatment alleviates Alzheimer’s disease symptoms in male mice
Researchers at the University of Chicago have demonstrated that the type of bacteria living in the gut can influence the development of Alzheimer’s disease symptoms in mice. Sangram Sisodia featured. (UChicago Medicine)
Addressing social needs and structural inequities to reduce health disparities
“Entering Asian American and Pacific Islander Heritage Month, a cutting-edge issue is addressing social determinants of health, which are especially critical among diverse Asian American ethnic groups that vary in education, income, and acculturation,” writes UChicago Medicine’s Marshall Chin. (NIMHD Insights)
Phage therapy to prevent cholera infections—and possibly those caused by other deadly bacteria
Discovered a little more than 100 years ago, bacteriophages, or phages, are generating renewed interest as potential weapons to fight bacteria that are resistant to multiple antibiotics. (The Conversation)
Common food additive found to affect gut microbiota
Experts call for better regulation of a common additive in foods and medicine, as research reveals it can impact the gut microbiota and contribute to inflammation in the colon, which could trigger diseases such as inflammatory bowel diseases and colorectal cancer. (ScienceDaily)
May 14, 2019 | Cancer
by Tim McGovern
Writer and editor based in Chicago
Remember The Blob? Even if you’ve never seen this 1958 B-movie classic, pop culture has likely introduced you to the concept: a shapeshifting mass that extends to swallow up and dissolve its enemies. This swallow and dissolve approach—on a microscopic level—is how white blood cells deal with infections. As Lev Becker, who specializes in these cells, explains: “These macrophages (their very name means ‘big eaters’) and neutrophils (the ‘first-responder’ white blood cells) are in every tissue in your body, and they play a fundamental role in maintaining your health, protecting you against infections from viruses or bacteria.”
Unlike the Blob and its strategy of indiscriminate destruction, white blood cells do a pretty good job of distinguishing the “good guys”—healthy human tissue—from the “bad guys”—viruses and bacteria. But sometimes they get it wrong. Becker goes on: “If they’re chronically incorrect—for instance, over-inflamed in the context of diabetes and heart disease, or under-inflamed in the context of cancer—long-term illnesses can result. And although we are looking at a variety of diseases, what unifies our lab is the philosophy and approach that one can either activate or inhibit the innate immune system to treat human disease.”
To understand how immune cell activity plays out in human disease, Becker and his team use an array of leading-edge techniques. “We always start with people,” he says, “and ask ‘What is different in the cells of people with and without a given disease?’ Then we work to find mouse models and cell systems that replicate that dysfunction.” This approach sets his lab apart from a more “traditional” approach: start with a molecule and learn everything about it in the cellular context, then—if it seems the molecule might play a role in disease—develop a mouse model, and finally, if the mouse results are promising, figuring out a way to ascertain the molecular activity in humans.
In Becker’s lab, “Every project has a human, mouse, and cell component to it.” It takes a novel assortment of tools to work in this way. In addition to the core biochemistry the team employs to parse the molecular pathways, they have developed new assays using cutting-edge computational techniques, with the goal of understanding the entire range of protein activity in a given cell. The capstone to all this molecular research is the lab’s ability to test their hypotheses not only in petri dishes, but in mice and human patients.
This ability to take research from human to molecule to human was always part of Becker’s plan: “My initial thought going into basic science versus medical science is that to impact health you have to take it one step further. Research scientists always hope that one day their findings will lead to treatments, but our focus on the translation part of research is especially important to us. We want to create medical interventions and develop therapeutics. That’s where we’re trying to go: start with humans, go back, find a molecule, take it to mice, and then launch a company, get funding, and move forward with actually developing and testing a therapy.”
A couple of years ago, leveraging the expertise and resources of the University’s Polsky Center for Innovation and Entrepreneurship, Becker launched Onchilles Pharma Inc. With seed funding from the George Shultz Innovation Fund, Onchilles is working to bring Becker’s research back to people, in the form of cancer immunotherapies which are more powerful, more precise, and better tolerated than current treatments.
Apr 30, 2019 | Cancer, Microbiome, News Roundup
A selection of health news from the University of Chicago and around the globe curated just for you.
Providing a community of support for young women
The region’s first pediatric lupus clinic opens at Comer Children’s Hospital thanks to the generosity of the Handley family and Lakeshore Recycling Systems. The clinic aims to help adolescents manage the physical and psychosocial challenges of living with lupus. Melissa Tesher featured. (Give to Medicine)
Drug delivery technique makes cancer immunotherapy more effective
Researchers in the Institute for Molecular Engineering at the UChicago have developed a new way to target immunotherapies and deliver them directly to tumors, helping to both reduce side effects and make the therapies more effective in treating cancer. Jeffery Hubbell and Melody Swartz featured. (UChicago Medicine)
Your sexual partners can change your microbiome, a new study in mice finds
People’s sexual partners could impact both their gut microbiome and their immune system, according to a new study from the University of Colorado, Denver. (STAT)
Gut microbiome directs immune system to fight cancer
Researchers identified a cocktail of 11 bacterial strains that activated the immune system and slowed the growth of melanoma in mice. Thomas Gajewski quoted. (Drug Target Review)
The Microbiome Center continues its focus on the broader world of microbes
Co-director Cathy Pfister, PhD, says the resources and research infrastructure being developed by the DFI are a tremendous boon for all researchers studying the microbiome at UChicago. The DFI’s emphasis on human health also allows the Microbiome Center to focus its efforts across many environments. (UChicago Medicine)
Apr 29, 2019 | Microbiome
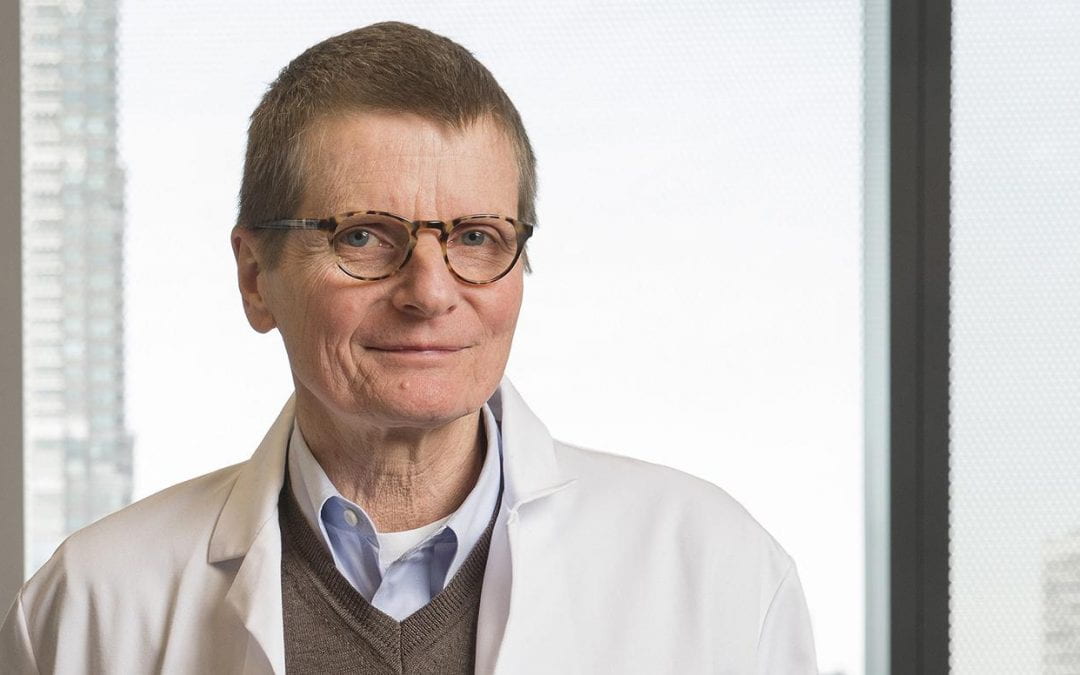
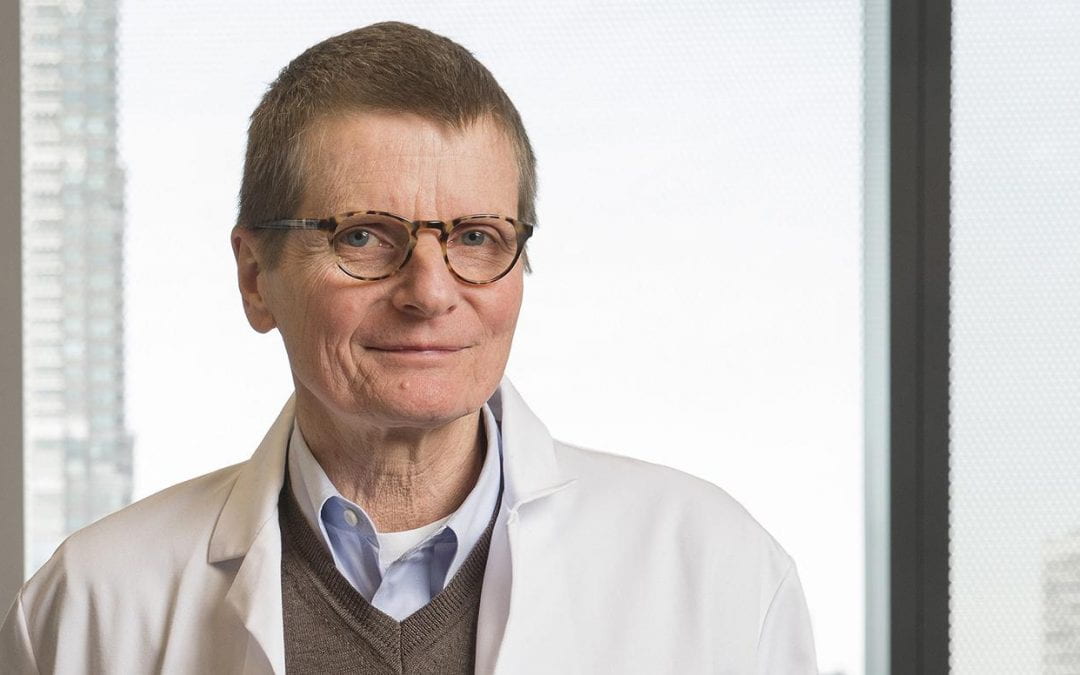
Following a national search, renowned physician-scientist Eric G. Pamer, MD, has been recruited to be the inaugural faculty director of the Duchossois Family Institute at the University of Chicago Medicine starting July 1.
Formerly with Memorial Sloan Kettering Cancer Center, Pamer will lead the Duchossois Family Institute as it seeks to carry out groundbreaking research on how the human immune system, microbiome and genetics may interact to maintain health. He will work closely with faculty, students and staff across the University of Chicago and UChicago Medicine to develop directions for research at the institute, to recruit outstanding faculty and to establish an innovative infrastructure that promotes discovery and translation.
The news comes nearly two years after UChicago Medicine announced the largest gift in its history to establish the Duchossois Family Institute: Harnessing the Microbiome and Immunity for Human Health. The institute is dedicated to investigating and developing new knowledge about the human biological defense systems, including the microbiome, and their therapeutic and commercial potential for preventing disease and maintaining lifelong wellness. The $100 million gift, announced in May 2017, was from Duchossois Group Inc. Chairman and CEO and longtime University and Medical Center Trustee Craig Duchossois, his wife, Janet Duchossois, and The Duchossois Family Foundation.
“We are delighted by the recruitment of Dr. Pamer, as it speaks to UChicago’s continued record of attracting the best minds who can take on great challenges,” said Kenneth S. Polonsky, executive vice president for medical affairs at the University of Chicago. “Under his leadership, the Duchossois Family Institute will leverage the university’s and medical center’s strengths and resources in the fields of genomics, the human immune system, data analytics and the microbiome to develop novel approaches to enhancing the body’s natural ability to maintain health and prevent disease.”
Pamer is an infectious diseases expert who specializes in immune defense against infections associated with cancer treatment and an accomplished scientist whose research focuses on the microbiome’s impact on resistance to a wide range of microbial pathogens. He comes to Chicago from Memorial Sloan Kettering Cancer Center in New York City, where he has served as head of the Division of Subspecialty Medicine since 2011 and director of the Lucille Castori Center for Microbes, Inflammation and Cancer since 2010. He joined Memorial Sloan Kettering in 2000 as chief of infectious diseases and has served as professor of medicine at Weill Cornell Medicine since 2001. Prior to his tenure in New York, he worked at Yale University from 1992 to 2000 as an assistant and associate professor of infectious diseases and immunobiology.
“My laboratory has been studying how to optimize the body’s immune defenses against a range of infections,” Pamer said. “Recent technical and computational advances have enabled us to investigate the role that commensal bacteria living on our surfaces and in the intestine play in defense against infections and in the pathogenesis of inflammatory diseases. We need to exploit these fundamental biological discoveries to advance the emerging field of health optimization and to identify how these insights can be applied, both clinically and commercially. I look forward to collaborating with researchers and clinician-scientists to tackle those challenges.”
Board certified in internal medicine and infectious diseases, Pamer is a member of the National Institute of Allergy and Infectious Diseases’ Board of Scientific Counselors and of the Bill and Melinda Gates Foundation’s Global Health Scientific Advisory Committee. He has published over 200 articles and book chapters. He received his medical degree from Case Western Reserve University and completed his residency and clinical fellowship at the University of California, San Diego.
Story originally appeared on The Forefront by UChicago Medicine

Apr 1, 2019 | Microbiome
by Folabomi Oladosu, PhD
Post-doctoral researcher specializing in pain and women’s health at NorthShore University HealthSystem
Holding a newborn for the first time simultaneously conveys the fragility of life and the enormous responsibility of ensuring this tiny person’s progression to adulthood. All the coos, gurgling, and late night cries are important steps in a newborn’s developmental process. These behavioral cues let us know that this baby is growing up exactly as she should.
Unfortunately, newborns born preterm—earlier than expected—are more likely to have developmental delays. Scientists are looking for ways to help reduce or eliminate some of these delays, and recent research indicates that the gut microbiome may be a key factor.
Before emerging into our messy world, a baby lives in an almost microbe-free environment. It’s during birth that most newborns are introduced to a great variety of helpful microorganisms, especially from her mother. The infant meets additional friendly bacteria as she nurses from her mother’s breast. These microbial partners begin teaching the baby’s immune system how to recognize friends—bacterial or chemical—and distinguish them from bad actors in the same way parents teach their children the difference between Aunt Mary and “stranger danger.”
Along with the immune-boosting proteins delivered via breast milk, these helpful bacteria give the newborn’s immune system the time and experience to learn and mature. In fact, most healthy, full-term infants show a pattern of progression where their gut microbiome evolves to look pretty much like an adult’s by about age two and a half.
But preterm newborns are different in several ways. They are more likely to be delivered via Cesarean section, a route that exposes infants to far fewer microbial allies. And because of their size and shortened development in utero, preterm infants usually need to stay in the hospital longer than most newborns, with reduced access to mom’s breast and the helpful microbes and immune-boosting proteins that come along with it. This means the baby’s immature immune system get less expert training and is thus more susceptible to infections.
To prevent these infections, preterm infants are often given antibiotics, a course that can set up additional problems. Antibiotics can kill bad guys but also destabilize the microbial community developing in the gut, interfering with the immune training that helps the baby thrive in the long run. It is thus important to understand the tradeoffs in using antibiotics and choose the best treatments for the long-term health of each little person.
Alyson Yee, a student in UChicago’s Medical Scientist Training Program (an integrated MD/PhD program) and then a member of the lab of Jack Gilbert (now at the University of California San Diego), wanted to consider that issue. “We think there’s a critical window in early life to train the immune system by being exposed to the right microbes,” said Yee. “For example, kids born by Caesarean section, with less exposure to microbes from their mother’s gut and vagina, have a higher lifelong risk for allergy and asthma. Childhood exposures to the environment, especially pets, can also change the microbiome and the immune system. This is why it’s so important to study the microbiome in infancy.”
Of course, the most sensitive infants are the tiniest. So Yee set out to analyze the gut microbiome of infants with very low birth weights by determining how their microbial profiles differed from full-term babies then examining how those differences affected weight and length gain during the first six weeks after birth. For a subset of those babies, she and her team were able to retest the children at two and four years of age.
Her team looked at two specific characteristics of the gut microbiome: the overall diversity, a sign of microbial health, and the rate of microbial turnover, a key measure of progress to microbial maturity.
At six weeks, the team found that very-low-birth-weight babies with greater microbial diversity who received a greater percentage of milk from their mother’s breast were gaining weight somewhat more quickly. But they also found that antibiotic exposure encouraged an abundance of proteobacteria, a kind of resistant microorganism commonly found in hospitals that can become opportunistic pathogens. Together with two other specific types of bacteria found in those on antibiotics, proteobacteria were correlated with poor weight and length gains. In contrast, infants with increased microbial turnover—including those delivered by C-section—tended to have fewer of these bacteria and grew faster during their hospital stay.
The best news is that microbial diversity in most of these very-low-birth-weight babies increased significantly over time. By age four, the baby’s microbial profile was very similar to that of her mom’s, proving yet again the resilience of the human organism.
It’s interesting to note that researchers have found similarities between the preemie microbiome and that of full-term infants who are undernourished—suggesting that therapies developed for one group may be helpful for the other.
Given the relatively small number of very-low-birth-weight babies they followed at six weeks (83) and at four years (25), the researchers suggest continuing expanded studies. UChicago neonatologist Erika Claud is already leading a major study that will follow of thousands of premature babies over five years to understand how the development of the microbiome affects childhood development and even school readiness. Stay tuned for more clarity on how we can promote the greatest health for our littlest fellow humans.

Mar 28, 2019 | Commercialization, Immunology, Microbiome, News Roundup
A selection of health news from the University of Chicago and around the globe curated just for you.
Polsky Center’s Life Science Launchpad partners with faculty to launch startups
The Launchpad bridges the gap between academic research and entrepreneurship by forming hands-on partnerships with life sciences researchers who seek to convert their research products into business ventures. Cathryn Nagler and Eugene Chang featured. (Polsky Center for Entrepreneurship and Innovation)
How the microbiome could be the key to new cancer treatments
The effectiveness of drugs that help the immune system fight cancer cells appears to depend on bacteria in the gut. (Smithsonian magazine)
Training cells to attack
Groundbreaking CAR T-cell therapy engineers cells to target tumors. Michael Bishop featured. (Chicago Health)
How to reduce the chances of being hospitalized for Crohn’s disease
Take these steps to lessen the risk of complications from the inflammatory bowel disease. David Rubin featured. (U.S. News and World Report)
Real innovation is going to be centered on how we collect, standardize, and harmonize data
Bridging the gap between clinical care and research means creating two-way collaboration, and improving the way in which data is collected, organized, shared. Sam Volchenboum featured. (Outsourcing-Pharma.com)
Mar 6, 2019 | Microbiome, Sustainability
by Elise Wachspress
Image courtesy of Regio Energie Solothurn
WellNews usually reports on groundbreaking research on the immune system, genetics, and the microbiome that promotes wellness—at the level of the individual.
Now for something totally different.
Laurens Mets is studying ancient microbes—archaea—as a way of improving human health for everyone in the world, banking on these tiny organisms to help clean up our environment, remove carbon dioxide from the air, and perhaps save the planet.
On the surface, archaea look something like bacteria, with similar shapes and no nuclei. But unlike bacteria, they have some genetic and metabolic similarities to plants and animals—and some traits that make them totally unlike either group. It wasn’t until 1977 that Carl Woese and George E. Fox proved archaea were a totally different domain, with their own separate, major branch on the “tree” of life.
The first archaea discovered were “extremophiles,” organisms that prospered in harsh environments like hot springs and salt lakes. Now they’ve been found everywhere, including in our own bodies. Archaea are amazing life-forms, in that they can live on a huge diversity of energy sources: ammonia, metal ions, even hydrogen gas. Some salt-tolerant types use sunlight as an energy source, and others can fix carbon from the atmosphere. They are particularly numerous in the oceans, and so far, none seem to be pathogenic.
Mets’s idea was to find and optimize archaea that would metabolize the garbage in our landfills and the carbon dioxide in the atmosphere—by-products of our own energy use—and then turn these into fuels. And he’s developed some proprietary strains of archaea (starting from some originally isolated from a hot spring in Iceland) that are already doing just that—in two different ways.
In the case of garbage, the approach is to “gasify” carbon-based trash (which is most of what fills our landfills) at extremely high temperatures, creating a mixture of largely hydrogen, carbon dioxide, and carbon monoxide. That part has been done by several other methods, but with an implicit problem: how do you manage the deadly carbon monoxide? Mets’s process uses archaea as a biocatalyst to turn the entire mixture—including the carbon monoxide—into methane. Methane makes up the bulk of what we call natural gas, a relatively clean fuel that is easily transported and stored through existing systems.
A new approach to carbon capture?
In the second approach, Mets uses archaea to solve two problems with solar and wind power. First, both generate energy as electricity, which currently meets less than 20 percent of the U.S.’s energy needs. Perhaps more important, solar and wind energy are intermittent, tough to store, and poorly matched to variation in demand over daily or yearly cycles. But Mets’s archaea can use energy from excess electricity to convert atmospheric carbon dioxide into methane. Switching from natural gas to electricity and back again would not only mitigate the variabilities in electricity production but also incentivize greater reliance on these renewable energy sources—and reduce net carbon emissions to the atmosphere.
With help from the Polsky Center for Entrepreneurship and Innovation, the University of Chicago has licensed out the early versions of Mets’s archaea technology to a German Company, Electrochaea GmbH. Germany and much of Eastern Europe, famously dependent on Russian fuel, recognize a crucial need for increased energy diversification. As Mich Hein, CEO of Electrochaea (and former entrepreneur in residence at the Polsky Center) pointed out in advance of last year’s Energy Storage Europe conference, the archaea technology can serve as “a drop-in replacement for fossil natural gas that can be stored or transported in existing natural gas infrastructure. The renewable gas product unites different energy sectors and provides economic leverage for owners and operators of existing assets.”
Electrochaea is now a partner in a venture called Store&Go that just opened a new plant in Switzerland, introduced by an absolutely charming spokesmodel: Archie, an archaea who demonstrates just how he cleans up after our own energy expenditures to make more fuels.
Mets, however, believes he can push the technologies much further. While he has developed the most energy-efficient strain of archaea so far, he is convinced that he and his lab can do better. These molecular geneticists want to advance experiments to iteratively select, mutate, and then sequence the genomes of the most carbon monoxide-tolerant archaea and develop microbes that are increasingly efficient at turning our carbon-based waste into storable, transportable fuel.
If archaea technology can create a closed loop for carbon-based fuels, where carbon uptake equals carbon emissions, the world may have reason to heave a sigh of relief. After the past decade of increasing global temperatures and dramatic variations in weather patterns—some costing cities and countries trillions of dollars—it is becoming clear that man-made climate change is threatening millions of lives around the world. Mets’s research (and yes, he is looking for funding support) holds the potential to save both money and the planet. These microbes could indeed help the entire world’s population—and all the other animals who live here—become healthier in many ways.
Elise Wachspress is a senior communications strategist for the University of Chicago Medicine & Biological Sciences Development office
Mar 4, 2019 | Neuroscience
by Folabomi Oladosu, PhD
Post-doctoral researcher specializing in pain and women’s health at NorthShore University HealthSystem
Every now and again, you wake up to find your arm or leg didn’t quite wake up with you. You dread it, but you wiggle through the pricking, tingling sensations until your once-numb limb is ready to start the day. What if, despite your best efforts, the numbness persists? Numb tingling limbs are one of several hallmark symptoms associated with multiple sclerosis (MS), an autoimmune disorder where the immune system attacks the central nervous system.
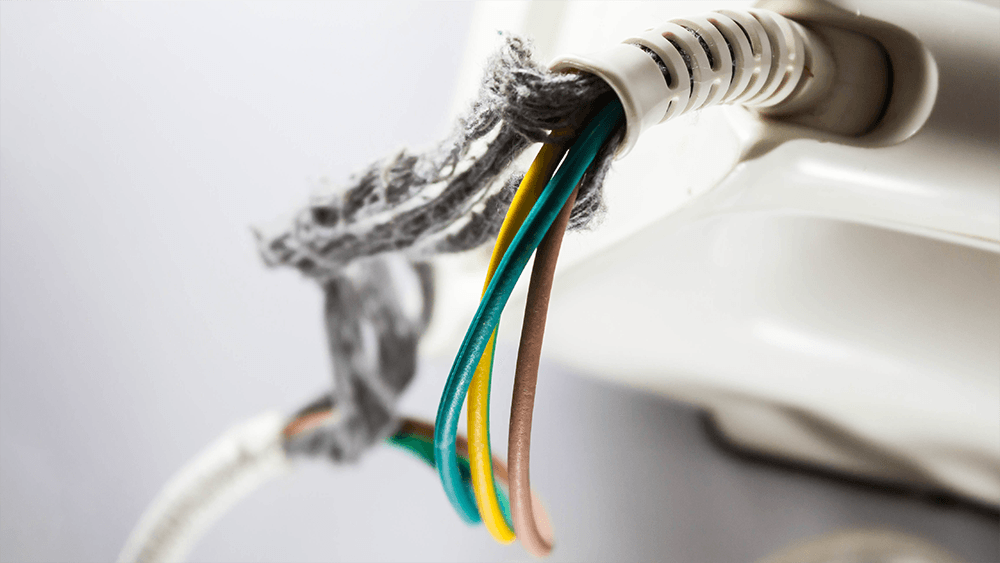
Our nerves are somewhat similar to an electrical power cable. The inside of a nerve is made of smaller nerve fibers. These fibers conduct important electrical signals and messages throughout the body. The outside of the fibers are covered by myelin, a fatty material formed by specialized brain cells. Thanks to its insulating properties, myelin speeds the transmission of electrical messages throughout the body.
If you bend any cable too often, eventually the outer plastic coating starts to fray, exposing the inner metal wiring. The cable may still work, but over time, it becomes less and less reliable (raise your hand if you’re on your third phone power cable). A similar phenomenon occurs in MS. The immune system attacks the body’s own cables, damaging the specialized cells and degrading the insulating myelin on nerve fibers. Over time, this demyelination produces a range of symptoms, including fatigue, depression, pain, and movement issues.
First-line treatments for MS aim to dampen the immune system to reduce demyelination. Although effective, these treatments make the body vulnerable to sickness and infection.
What if there was a way to directly protect the cells and the myelin they produce? Brian Popko and his team wanted to know if Sephin1, a small molecule that enhances a cell’s defensive response to environmental stressors, could protect nerve fibers from demyelination.
Popko uses a mouse model where an injection of myelin proteins coupled with a toxin generates an immune response similar to that in MS patients, initiating a MS-like disease in mice. He and his team then injected the mice with Sephin1 and followed the mice’s responses for 35 days. In this mouse model, clinical symptoms usually appear after 11 days and peak on day 17. When given one week after the initial injection to create MS-like symptoms, Sephin1 delayed disease progression, with clinical symptoms peaking on day 26.
The findings suggest that Sephin1 delayed disease progression by boosting the defensive response to insults from the immune system. When compared to control mice, mice that received Sephin1 had more of the specialized brain cells and less demyelination in the spinal cord on day 17. Sephin1 also dampened immune cell activity in the spinal cord.
The team went on to discover that Sephin1 worked even better when it was paired with interferon beta (IFN-β), an anti-viral protein native to the body, also used as a common treatment for MS. Mice that received both Sephin1 and IFN-β showed much slower, less severe disease progression.
This timely translational research from the Popko lab illustrates the promising therapeutic effects of Sephin1 for MS, especially when combined with IFN-β. Its demonstrated efficacy in MS mouse model indicates Sephin1 may help to protect indispensable nerve fibers from demyelination in MS patients. Dr Popko is currently exploring opportunities to assess the therapeutic safety of Sephin1 for MS patients.
Feb 27, 2019 | News Roundup
A selection of health news from the University of Chicago and around the globe curated just for you.
Germs in your gut are talking to your brain. Scientists want to know what they’re saying.
The body’s microbial community may influence the brain and behavior, perhaps even playing a role in dementia, autism and other disorders. Sam Sisodia featured. (New York Times)
At the Forefront Live: Head and neck cancer
Medical oncologist Alexander T. Pearson and nurse navigator Patricia Heinlen discuss head and neck cancer, including the HPV vaccine and how new treatment approaches are tailored to each patient’s cancer type, making treatments more effective while reducing side effects. (UChicago Medicine)
Teaching our immune system how to fight cancer
UChicago researchers work to make the next leap in cancer immunotherapy, in which the immune system is stimulated to fight cancer. (UChicago News)
‘Cultured’: A look at how foods can help the microbes inside us thrive
A surge in microbiome research over the past two decades has revealed microbes do much more than simply digest food. They can mediate weight gain, fight off infection, and even alter our mood. (NPR)
Microbiome research will accelerate the biotechnology industry
Humans have relied on the ocean for millennia as a source of food and materials for tools. Now, we rely on the ocean as a source of genes that we can harness to increase food stocks and use as medicine for cancer and other diseases. (Forbes)

Feb 14, 2019 | Microbiome
by Folabomi Oladosu, PhD
Post-doctoral researcher specializing in pain and women’s health at NorthShore University HealthSystem
At the start of your doctor’s visit, as the nurse checks your pulse and blood pressure, you probably take slow deep breaths, trying to convince your doctor and yourself that you’re cool, calm, and collected. (No? Is that just me?)
Your blood pressure can tell your doctor a lot about you—including your risk for peripheral arterial disease, or PAD. In PAD, arteries that carry blood throughout the body are narrowed by deposits of fat and cholesterol. The disease is common, with more than three million new cases surfacing every year. PAD puts people at increased risk of both heart attack and stroke, so it’s important to treat it quickly and effectively.
When diet, physical activity, or medications are not enough, surgery is the next step to open up the narrowed arteries. Options include an angioplasty, where a tiny balloon is inserted into the blocked artery. The balloon is inflated to crush the plaque deposits and then removed to restore blood flow.
Following surgery, these once clogged arteries should carry red blood cells throughout the body like an amusement park water slide. To your dismay, you find this water park attraction might need more repairs three to 12 months later because of restenosis, the abnormal re-narrowing of arteries following surgery (Get it? Re-stenosis). Restenosis occurs in about 40 percent of patients after angioplasty and is usually treated with yet another surgery.
What causes this re-narrowing? Inserting the balloon and compressing the plaque may cause a mild arterial injury. The immune system responds, sending in white blood cells and platelets to repair the artery. But sometimes the immune system goes overboard and causes scarring instead. This means that the same arteries that were first narrowed by fatty deposits are narrowed yet again because of scarring caused by the immune system.
Why does the immune system to go into hyper-drive following surgery? One contributing factor may be—amazingly—the bacteria living in our gut. Drs. Eugene Chang and Betty Theriault of the University of Chicago collaborated with Dr. Karen Ho of Northwestern University to investigate the role of the gut microbiome on arterial healing following surgery.
Using their extensive knowledge and technical expertise, the team developed a method to study arterial healing in germ-free mice, mice with no gut bacteria. Their work revealed that germ-free mice developed much less arterial scarring following surgery compared to normal mice. Their research also showed that the immune system of germ-free mice was different than normal mice, using different white blood cells less likely to encourage swelling and scarring at the injury site.
All of us have been surrounded by germs since the day we were born. So if we need an angioplasty, we’d be like those normal mice, more likely to have arterial scarring after surgery.
Is there anything we can do to prevent restenosis? Related work by Drs. Ho and Chang suggests yes. A month-long treatment of the antibiotic vancomycin paired with sodium butyrate (a compound that slows cell growth) reduced arterial scarring in rats following an angioplasty. Legumes like beans and peanuts, when digested by gut bacteria, are a common source of sodium butyrate. This suggests that the dietary changes prior to angioplasty may help reduce arterial scarring and restenosis.
This “basic science” research by Drs. Chang, Theriault, and Ho provides great insights for better health. It shows that, despite their microscopic size, gut bacteria can greatly influence how we heal from common surgeries. The humble legume–cheap, tasty, easily stored, and environmentally friendly to grow—may help to keep our internal water slides open for service long after initial repairs.