Auto text: “Insert Ellipse Oriented” or “Insert Ellipse Unoriented”
If a suspected melanoma case comes for frozen section – please check with attending prior to freezing!
Skin excisions received for permanent section are most often for cutaneous Carcinoma (Squamous, Basal, Merkel) or Melanoma. This guide can be applied to lesions of many types. Specific instructions for melanoma are given (if applicable) within the text below.
Triage
- Measure skin in 2 dimensions and depth of excision.
- Measure & describe any lesions/ulcerations present on the epidermis, and closest extent to skin margins.
- Pin out large elliptical or trapezoidal specimens on wax, in order to prevent edges from curling. Make sure to place gauze between the wax and the specimen.
- Melanoma: Excisions should be fixed overnight!
- Non-Melanoma: Generally should fix overnight unless small and thin.
Gross
- Ink the deep and peripheral resection margins.
- Unoriented excisions: Ink the deep and peripheral margins ONE color.
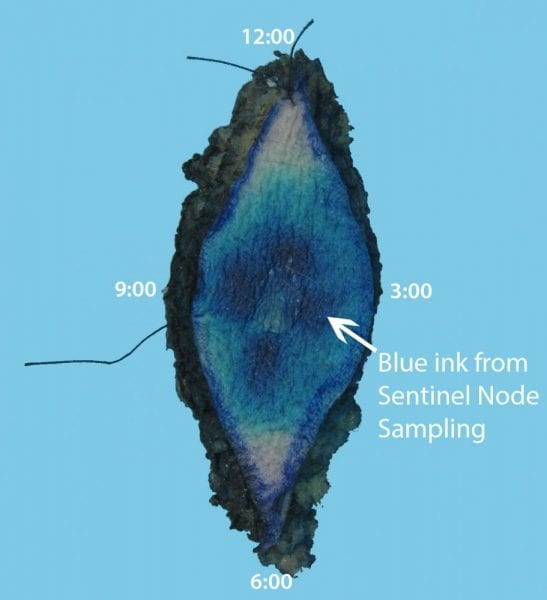
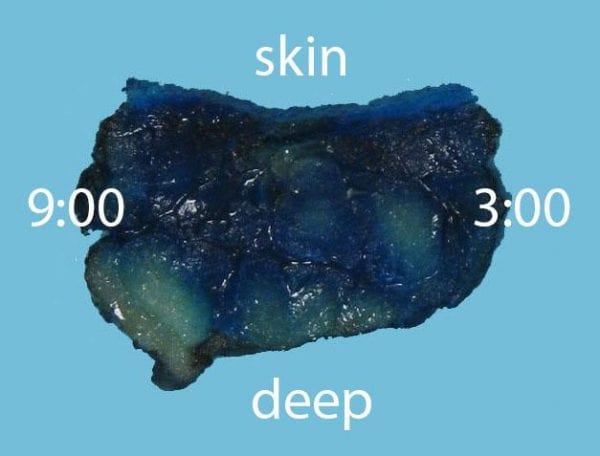
- Oriented excisons: Identify the marking suture and orient the specimen accordingly using anatomic position. If anatomic position is not known, orient using clock face. Ink the resection margins in TWO colors: Visually separate the specimen parallel to the long axis. Ink one half blue (3:00 half, for example) and one half black (9:00 half, for example), meeting the colors in the middle. Be sure to include both the deep surface and peripheral edges in your ink.
- If tips are narrow: amputate (no smaller than 3-4 mm deep), bisect perpendicular to margin, and submit.
- If tips are wide: amputate and serially section perpendicular to margin.
- If the specimen is small and you will submit it entirely, also submit the tip sections entirely (2-3 pieces per container).
- If the specimen is large and you will NOT submit it entirely, submit only representative sections of the tips (including closest of tumor to margin, 1-3 pieces per container).
- DO NOT SUBMIT EN FACE TIPS FOR SURG PATH CASES unless discussed with attending first.
- Serially section the remaining portion perpendicular to the long axis. Inspect all cut surfaces to look for tumor nodules, scar, or pigmentation. For melanomas, cases with >2 mm depth or >2 mitoses/mm2 on biopsy have increased risk of satellite nodules. Check the biopsy and look for satellite nodules!
- Measure in 3D and specify the gross depth of invasion. Describe any grossly visible lesion, including closest extent to deep and peripheral resection margins.
- For primary excisions (not recurrences, see below):
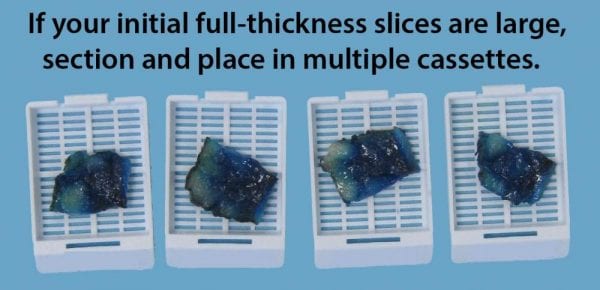
- If the overall specimen is small (2-3 cm in greatest dimension): Submit the entire specimen, including the lesion. Place no more than 1 piece into each cassette.
- If the overall specimen is large (>3-4 cm in greatest dimension), submit representative lesions (~ 1 section per cm for each lesion) including nearest margin and interface with skin/surrounding tissue. Place no more than 1 piece into each cassette. Discuss with attending if unsure!
- For re-excisions, recurrences, and post-treatment specimens: This procedure may be done for epithelial, melanocytic, or mesenchymal tumors with positive or close margins.
- If lesion is not grossly visible: submit all of the tissue involved by scar / prior biopsy site. Submit any additional suspicious areas (included pigmented areas in the case of melanomas). Submit representative normal on either side of biopsy site.
- If lesion is grossly visible: submit ~1 section per cm of greatest dimension of lesion.
- If unsure, please consult the attending!
- If specimen has subcutaneous tissue greater than 1.0-1.5 cm, place cassettes on FATS processor run.

